Labour and delivery are unique experiences in a woman’s life. If not dealt with well, it can lead to unpleasant experiences and mental agony.
Society punished women by denying them the right to a pain free delivery for a very long time, until the breakthrough in 1853, when Sir John Snow first gave Chloroform to Queen Victoria for the birth of her 8th child Prince Leopold.
Labour is a complex and highly individual process, not every women wants or needs analgesia (pain relief) for delivery. Educating the women during the course of pregnancy, whenever possible is the best option for helping them to make an informed decision. The decision to receive any form of pain relief is personal and should be made by the patient.
The optimal pain relif for labour is one that can provide pain relief for first and second stage of labour with minimal effects on mother and baby. The ideal technique should provide effective and rapid onset of pain relief with minimal muscle paralysis, long duration, minimal risk of material toxicity and minimal placental transfer and effects on the baby.
Neuraxial labour analgesia (epidural, spinal or combined spinal - epidural analgesia) is currently the most effective method of providing labour analgesia.
Its a method of pain relief for delivery which abolishes the pain without interfering with the uterine contractions which are necessary for the expulsion of the fetus.
Attempts to minimize the pain of labour non-pharmacologically first began in the early 20th century. It was suggested that the pain of child birth was brought about by fear and tension and recommended passive muscle relaxation to reduce the pain.
Psychoprophylaxis is a technique which involves educating the mother about the functioning of her body and the physiology of labour. Other techniques involve simple emotional support from the patient’s partner or another labour companion, touch and massage, the application of hot or cold compresses and hydrotherapy.
Some techniques require fairly extensive preparation and antenatal training. These include Biofeedback, Acupuncture, Hypnosis and Transcutaneous nerve stimulation (TENS). TENS involves the application of a variable electrical stimulus to the skin at the site of pain . Great or considerable relief of labour pain is seen in 20-24% of mothers with about 60% having slight relief.
All drugs given systemically will cross the placenta to reach the baby to some extent.
Pethidine is the most commonly used opiate in obstetric practice. Intramuscular pethidine 100mg or 150mg was deemed satisfactory by only 22.4% of women in first stage of labour and in 47.7% it gave no relief at all. Nausea and vomiting occur in 50% of patients and exerts both immediate and long term effects on baby.
Morphine is a powerful opiate to pethidine. It benefits from the ability to allay anxiety and longer duration of analgesic action but frequently causes nausea and vomiting and is a potent depressor of baby.
Benzodiazepines are used for maternal sedation. Most commonly used benzodiazepines ia Diazepam but has side effects on baby which includes decreased muscle tone, decreased activity, respiratory depression . Now a days benzodiazepines are not indicated for pain relief during pregnancy
Pentazocine ( commonly known as fortwin ) is popular drug( medicine) and obstetricians commonly use it because when used in multiple doses does not produce much changes in the Apgar scores in babies as compared to pethidine. In addition the fetal heart rate is not so affected by pentazocine as it is with pethidine. The chief drawback of pentazocine is unpleasant hallucinogenic side effects and the limited pain relief that it can produce.
Ketamine has been used to produce analgesia during labour, doses in the range of 0.25mg/kg reportedly produce effective analgesia without any adverse effect on uterine blood flow, uterine activity or neonatal status.
Inhalational agents are anaesthetic gases which the labouring women has to inhale(smell) periodically to get pain relief.
Trichloroethylene commonly causes nausea and vomiting and its sweet smell may be unpleasant. Its use in labour is now uncommon.
Analgesia produced by Methoxyflurane persists into the period after inhalation ceases. Nausea and vomiting are uncommon and although inorganic fluoride concentrations are increased in both mother and infant, the risk of renal damage seems negligible as long as inhalation is restricted to low concentrations for limited periods. Again its use in labour is now uncommon.
Entonox which is 50 : 50 prepared mixture of nitrous oxide and oxygen is employed as a self administered intermittent inhalation which if used in the correct manner can produce acceptable levels of analgesia. It should be possible for 40 - 82% of mother to obtain substantial benefit from Entonox when properly managed by the staff.
Peripheral nerve blockade means blocking of the nerve fibers at the periphery which supply the uterus.
Paracervical block can be of value in the first stage of labour. It provides successful analgesia in approximately 80% of mothers. However in the first few minutes after initiating a block a high incidence of fetal bradycardia (decrease in heart rate) associated with a falling pH and oxygen tension have been seen. It has been suggested that the block should be administered in well spaced stages in order to minimize these effects. This complication has led to a marked diminution of its use worldwide.
Pudendal nerve block is almost always used to facilitate operative vaginal delivery and is usually performed by the obstetrician. Local infiltration of the perineum may be necessary because bilateral pudendal nerve block was not totally effective in nearly 50% of cases.
Lumbar epidural blockade is currently the gold standard for pain relief in obstetrics. Epidural analgesia provides the most effective form of pain relief devised so far for labour and delivery. The establishment of an epidural service requires committed individuals and the presence of an anaesthetist in the labour ward, as well as equipment and staff education.
Caudal extradural block is useful in the late first stage and second stage of labour. It provides good relaxation of the perineal muscles. Problems include a relatively high forceps rate, attributed to abnormalities of rotation of the fetal head due to relaxation of the pelvic floor.
Single shot spinal have limited utility in early labour and are more useful in the second stage of labour. It is an easier block than epidural blockade and provides good relaxation for the pelvic musculature. Disadvantages cited include post dural puncture headaches. However its incidence is low with the use of fine pencil point (26 or 27G) needles.
Since the introduction of this technique in the early 1980’s it has gained increasing popularity for analgesia and anaesthesia in labour and delivery. Because CSE allows for ambulation of the parturient it has been called the Walking Epidural.

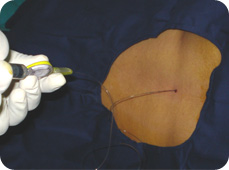
The epidural space lies just outside the special covering or dura, which encloses the spinal canal. An 'epidural' is a type of regional anesthesia in which a needle is positioned between the bones of the spine to allow the anesthesiologist to insert a small plastic tube (or catheter) into the epidural space. The needle is then removed and local anesthetic is injected through the catheter. This local anesthetic moves (or diffuses) across the dura. into the spinal canal, and temporarily stops the spinal nerves from working, so that sensation and movement in the area supplied by the nerves does not occur. When the effect of the local anesthetic wears off, sensation and movement will return. If a weaker solution of local anesthetic is used, then only painful sensations will be blocked. This is very useful for controlling pain and is called epidural analgesia. Often continuous infusions of local anesthetic solutions are used, which allows the effect to be maintained as long as required. . This is a very useful and safe procedure, when performed with appropriate care by an experienced anesthesiologist.
In obstetric units where successful epidural service is established almost any medical or obstetric complication may be regarded as an indication for regional analgesia. This is largely because it may be desirable to avoid both the stress of painful labour and the risk of general anaesthesia should operative delivery be necessary.
It is a single most important indication for epidural analgesia, which not only provides physiological benefits to both mother and baby but also makes a labouring women more comfortable, less fatigued and therefore more cooperative.
Pregnancy induced hypertension is the commonest obstetric indication for epidural analgesia. Epidural blockade is of little value in the absence of pain but in labour it has generally been found to control hypertension successfully and better than hydralazine and magnesium sulphate (commonly prescribed medicines for contol of blood pressure in pregnancy). Epidural analgesia produces favorable hemodynamic changes and a consistent improvement in blood flow to the baby. Complete analgesia could minimize the chance of fits assosiated with pregnancy induced hypertension . Moreover general anaesthesia that is particularly risky in the presence of edema of face can be avoided.
These patients have increased chances of having complication during labour. Epidural pain relief can minimize the adverse effect of increased blood supply to the heart (which should be avoided in these patients) due to pain or anxiety
Epidural analgesia is of benefit in chest disease because it avoids increases in respiratory rate associated with painful contraction.
Trial of labour means giving a trial for normal delivery in patients who have undergone caesarean section previously. Epidural analgesia in no way masks the danger of scar rupture . The pain from the scar and pain from the uterine contractions are felt at the same site and the scar is most likely to be stressed during a contraction. Epidural local anaesthetic more readily blocks the pain of uterine contraction than pathological pain, so that it may aid in the diagnosis of scar dehiscence. Analgesia given early in these patients may reduce maternal exhaustion and can subsequent1y be converted to epidural anaesthesia in case a caesarean section is warranted.
If an epidural catheter is already insitu, in the event of fetal distress or any need of caesarean section; it can easily be converted to anaesthesia by simply altering the dose of the drug, and the position of the patient, thus, saving time and effort.
Epidural analgesia is associated with reduced neonatal mortality rate among low birth weight babies Likewise the outlook in twin pregnancy particularly for the second twin is improved.
By decreasing the catecholamine (adrenal hormone) secretion associated with labour pain, epidural block can improve uterine contractility and rhythmicity and is especially indicated in cases of incoordinate uterine action.
Preterm fetus, Breech Presentation & Multiple Pregnancy - In these conditions an epidural block allows a more controlled delivery because of relaxed pelvic floor muscles and a decreased urge to push.
It is evidenced following vaginal delivery under epidural block as compared to delivery without epidural block This can be explained by the epidural induced peripheral pooling of blood in legs and thus decreased cardiac output.